You've all heard of dehydration , but do you really know its consequences ? Can you actually recognize the effects of dehydration on your body? We'll find out more in this article!
It's true that we often feel thirsty, but it's important to hydrate before that feeling appears, as it's already a sign of dehydration ! Furthermore, this sensation may not appear at all or may disappear after a while. It's therefore possible to forget to hydrate, in which case dehydration can worsen. That's why it's crucial to ensure children and the elderly stay well-hydrated, especially during the summer.
The first symptoms are usually subtle : headaches , fatigue, dizziness, and confusion. Sometimes you only realize you have a headache after a long day without drinking enough water, and these sensations disappear when you rehydrate.

The evolution of the weight curve is very important. Indeed, weight loss is one of the indicators of dehydration to consider:
- Mild dehydration , corresponding to a loss of 1 to 2% of body weight , leads to a decrease in physical and cognitive performance of 10 to 20%. Fatigue then sets in gradually, and a sensation of thirst may appear, although it is sometimes absent. Physical signs such as dry mucous membranes , dark circles under the eyes , and cold extremities may be observed.
- Moderate dehydration , corresponding to a loss of 2 to 4% of body weight, manifests as increased fatigue and decreased alertness. The heart rate increases to compensate for the reduction in blood volume, resulting in tachycardia. The sensation of dry mouth intensifies, the skin becomes duller, and a temporary skin fold may appear when lightly pinched.
- Severe dehydration , corresponding to a loss of 5 to 8% of body weight , causes impaired consciousness ranging from disorientation to confusion. The decrease in blood volume leads to hypotension and an increased risk of serious events, such as fainting or falls. The skin becomes dry , skin folds persist, the cheeks become sunken, and urine production decreases significantly (oliguria).
When fluid loss reaches 8% or more of body weight, the situation becomes critical and constitutes a clinically serious case. The risk of coma is high , organs begin to malfunction, and the limbs become cold to the core—a sign of impending circulatory shock.
What is dehydration?
Dehydration results from an excessive loss of water and minerals that is not replenished by fluid intake. Since water is essential for many bodily functions, a lack of it causes the effects described above.
There are several types of dehydration: extracellular dehydration , intracellular dehydration , and global (or chronic) dehydration . These types of dehydration share common effects and have more specific signs that allow them to be distinguished.
Whatever form it takes, dehydration should never be taken lightly. Insufficient hydration can quickly affect vital functions and endanger your health.
Most common causes of dehydration
Dehydration can have multiple origins, and its causes are often similar.
First, there are kidney losses . These can be due to excessive diuresis (the volume of urine excreted in 24 hours), which is found, for example, in the case of diabetes . Certain kidney failures or the use of diuretics can also lead to significant fluid loss.
Digestive losses are also a common cause of dehydration that must be addressed promptly. Prolonged diarrhea and vomiting lead to a rapid loss of water and electrolytes , which can result in severe dehydration if fluid intake is not quickly replaced.
Skin losses are often underestimated. Yet, excessive sweating during physical activity or in hot weather is a major cause of dehydration. Fever and heatstroke also increase fluid loss.

Pulmonary losses , although less visible, can contribute to dehydration, as a quantity of water is expelled as vapor. This phenomenon is exacerbated in cases of hyperventilation , particularly during physical activity, contributing to the loss of body water.
Other external factors can contribute to dehydration , and excessive alcohol consumption is a prime example. Alcohol reduces kidney function, leading to increased urination as a compensatory mechanism.
What are the symptoms of dehydration?
Dehydration can affect different parts of the body, resulting in varied symptoms depending on whether it is extracellular or intracellular.
Symptoms of extracellular dehydration
What is this ? Extracellular dehydration results from a loss of water at the extracellular level (plasma and interstitial fluid). While the intracellular water volume remains the same, an effective extracellular osmotic pressure is maintained.
Extracellular dehydration initially manifests as significant fatigue, loss of appetite , and an absence of thirst, which can delay fluid intake and worsen the condition. Unlike intracellular dehydration, the mucous membranes remain moist, but slight weight loss may occur due to a decrease in plasma volume.
Clinical examination reveals flat peripheral and jugular veins, as well as cold and discolored extremities , indicating low central venous pressure. Hypotension develops, causing dizziness and a rapid pulse to maintain adequate organ perfusion. Skin tone is altered, with persistent skin turgor, particularly in the abdomen, subclavicular region, and inner thighs (this sign can, however, be difficult to interpret in the elderly).
The eyeballs appear sunken, a sign of some fluid deficiency. In cases of severe extracellular dehydration, the clinical condition worsens with very low blood pressure (below 80 mmHg), cold extremities, and mottling of the skin, indicating an imminent state of shock requiring urgent medical attention.
What are the risks? Severe extracellular dehydration can lead to a significant drop in blood pressure, limiting oxygen supply to the organs and causing hypovolemic shock. The kidneys, lacking water, drastically reduce urine production or risk acute renal failure . Without prompt treatment, these complications can be life-threatening. Therefore, we advise you to make an appointment with a healthcare professional as soon as possible!
Symptoms of intracellular dehydration
Intracellular dehydration occurs when the intracellular compartment becomes dehydrated due to an increase in plasma osmolarity (generally an excessive concentration of sodium in the blood). The body compensates for this by releasing water from the intracellular compartment into the plasma to dilute the excess sodium and thus restore fluid balance . This loss of intracellular water leads to cell contraction, particularly affecting brain and muscle cells.
One of the first signs of intracellular dehydration is intense and uncontrollable thirst , as the body desperately tries to compensate for the fluid deficit. As the situation worsens, altered consciousness develops, ranging from confusion to a deep coma in the most extreme cases.

Weight loss can be significant, reaching up to 20% of body weight, a sign of severe dehydration. This dehydration is often accompanied by fever and rapid breathing, which exacerbates the fluid loss.
Other signs can help identify this form of dehydration. The mucous membranes are dry and the tongue is retracted. A medical examination may also reveal neurological problems, a direct consequence of the shrinkage of brain cells.
What are the risks? Severe intracellular dehydration can have serious effects , especially on the brain . When cells lose too much water, they shrink, which can cause memory problems, difficulty concentrating, and confusion. In the most serious cases, this can lead to loss of consciousness or a coma.
In infants and the elderly, the brain is more fragile, and this dehydration can sometimes cause a small cerebral hemorrhage (subdural hematoma). If it lasts too long, it can leave lasting effects on intellectual and motor skills.
How to treat dehydration?
Adult, child, infant: a different treatment?
To rehydrate , the principle is the same for everyone: drink to replace lost water and restore electrolyte balance . However, the method of administration and management vary depending on age and the severity of dehydration.
For an infant, for example, oral rehydration solutions (ORS) are necessary. These solutions, specifically designed to replenish lost fluids and electrolytes , are the best option because babies have difficulty expressing their thirst and cannot regulate their own hydration.
For an older child, rehydration can be achieved through oral rehydration solutions (ORS ), but also through diet with electrolyte-rich foods such as salt (sodium) or bananas (potassium) . However, getting them to drink large quantities of water can be difficult. If dehydration is mild to moderate, encouraging them to drink small amounts frequently is an effective approach. If the child refuses to drink plain water, alternatives such as lightly sweetened and salted drinks, broths, or water-rich fruits (watermelon, cucumber, etc.) can be used.
For an adult, all methods are suitable, and it is easier for them to assess their condition and measure their water intake. However, severe dehydration should not be ignored and may require urgent medical attention!
What are the solutions?
Severe cases and intravenous solution
If severe dehydration is suspected, consulting a doctor or going to the hospital is essential. In terms of treatment, there are several options: first, directly controlling the amount of fluids needed. Indeed, controlled oral rehydration, under medical supervision, is necessary to prevent any osmotic imbalance.
Then, in the worst cases (repeated vomiting, altered consciousness, hypovolemic shock…), it is possible to resort to the intravenous administration of a sodium chloride solution.
SRO
Oral rehydration solutions (ORS) are the gold standard for treating mild to moderate dehydration, particularly in infants and young children. Recommended by the WHO , they allow for rapid absorption of water and electrolytes thanks to the combination of sodium and glucose. They are especially effective in cases of diarrhea, gastroenteritis, or fever, when the child loses a significant amount of fluid.
In adults, rehydration relies primarily on regular water consumption, including drinks containing sodium, potassium, and glucose to improve intestinal water absorption and fluid retention. Several solutions exist, from the most basic, such as sweetened and salted water, to those that optimize the body's effects with additional supplements, like trace elements, as offered by Hydratis.
Why use Hydratis?

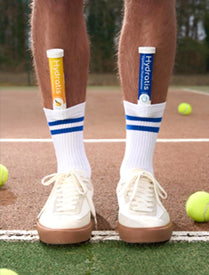
Hydratis is a hydration solution composed of sugars, electrolytes, and trace elements, designed to improve hydration in cases of fatigue , intense physical exertion , hot climates , or athletic recovery. It is based on WHO recommendations and suitable for a wide range of people.
Its convenient format and different flavors, to suit everyone, make it a pleasant alternative to classic solutions, while offering fast and targeted hydration.
5. Some tips to prevent dehydration
To prevent dehydration, there are two main conditions to respect:
First, ensure you maintain a good electrolyte balance . This can be done simply with a varied diet, or with ORS (oral rehydration solution).
Next, it's essential to drink enough water , beyond simply listening to your thirst. This is especially important for vulnerable individuals (young people who may have difficulty assessing their condition or quenching their own thirst, and the elderly, for whom the effects of dehydration are amplified) and for athletes, who lose water much more quickly through perspiration and exhalation. Oral rehydration solutions (ORS) like Hydratis are ideal in this case, and they also come in various flavors. If you prefer to use tap or bottled water, ANSES (the French Agency for Food, Environmental and Occupational Health & Safety) offers a helpful infographic to highlight the key points.
Bibliography
Bottled water or tap water: good consumption practices - ANSES
Adrogue, HJ, & Madias, NE (2000). “Hypernatremia”. New England Journal of Medicine, 342 (20), 1493-1499. https://pubmed.ncbi.nlm.nih.gov/10816188/
Hew-Butler, T., Rosner, MH, Fowkes-Godek, S., et al. (2008). "Exercise-Associated Hyponatremia: Consensus Guidelines". Clinical Journal of Sport Medicine, 18 (2), 111-120. https://pubmed.ncbi.nlm.nih.gov/26102445/
Cheuvront, SN, Kenefick, RW, & Sawka, MN (2010). "High Sweat Sodium Losses: A Risk Factor for Cramping and Hyponatremia?". Journal of Athletic Training, 45 (1), 25-30. https://pmc.ncbi.nlm.nih.gov/articles/PMC9699060/
Sawka, MN, Cheuvront, SN, & Kenefick, RW (2015). "Hypohydration and Human Performance: Impact of Environment and Physiological Mechanisms". Sports Medicine, 45 (S1), 51-60. https://pubmed.ncbi.nlm.nih.gov/26553489/